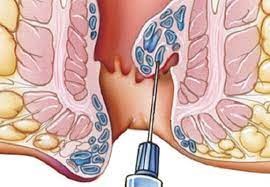
A hemorrhoidectomy is surgery to remove internal or external hemorrhoids that are extensive or severe. Surgical hemorrhoidectomy is the most effective treatment for hemorrhoids, though it is associated with the greatest rate of complications. Types of hemorrhoidectomies and related procedures performed during surgery:
Closed Hemorrhoidectomy
Open Hemorrhoidectomy
Stapled Hemorrhoidectomy (Procedure for Prolapse and Hemorrhoids - PPH)
Rubber band Ligation
Lateral Internal Sphincterotomy
After surgery
You will be able to eat and drink on return from theatre, the nurse will be checking your vital signs and wound. The nurse will advise what time you will be discharged. You should have someone to escort you home and a responsible person to stay with you overnight.
Preventing further/future problems with haemorrhoids
There is no guaranteed way of preventing haemorrhoids coming back after your surgery. Ensuring adequate fibre in your diet is a good place to start, this will reduce the risk of constipation and the straining to pass a stool that can cause haemorrhoids.
General recommendations are:
• Try to include high fibre foods at each meal throughout the day
• Choose wholegrain cereals e.g. wholemeal bread and wholegrain/high fibre breakfast cereals or porridge.
• Eat at least five portions of fruit and vegetables per day. Remember to eat the skin where possible.
• Include pulses e.g. peas, beans and lentils at meals. Add themto soups, stews and casseroles.
• Ensure you drink plenty of fluid – six to eight glasses per day.
Relatives/carers
The waiting area and Surgical Day Unit are for patient use only, therefore your relative/carer will not be permitted to stay with you. You can discuss this at any time with the nurse in charge.
There are no visiting hours within the unit. However, relatives and carers are welcome to use the dining and restaurant facilities, and free WiFi, which are available in the Golden Bistro and coffee shop on level one.
Discharge advice
• Slight staining from your wound may continue for a few days –wear a small pad to protect your underwear.
• Continue to take the painkillers given to you on discharge.
• You may experience some discomfort for 24-48 hours.
• When you move your bowels, avoid straining.
• If given laxatives to take home, continue to take these as advised.
• Daily baths will help with pain relief and keeping your wound area clean.
• Continue with your normal diet but remember to include fibre rich foods.
• You will have antibiotics to take to reduce infection – please complete the course prescribed to you.
You may be discharged the same day. If you have to remain overnight please make arrangements for discharge for 10am. The nurse will advise you if you have to stay longer.
Rest this evening and avoid strenuous activities.
In the next 24 hours, you must not:
• drive;
• drink alcohol; or
• use machinery.
Take your usual medications and any that you may have been given by the nurse today. It is normal to feel some pain after surgery. You will be prescribed and given regular painkillers during your stay in hospital. On discharge from hospital you will be given painkillers to take home.
Routine follow-up is not usually required.
Contact your GP if:
• You have severe pain not relieved by medication.
• You have excess bleeding from the wound site.
• You have extreme redness or swelling around the wound site or drainage of pus.
• You are unable to pass urine.
• You have continual vomiting.
• You have a fever. Severe pain or bleeding are rare complications.
In the event of an emergency, you should go to your nearest Accident and Emergency Department.